
What Does D SNP Stand For? A Comprehensive Guide for Dual Eligible
March 2, 2024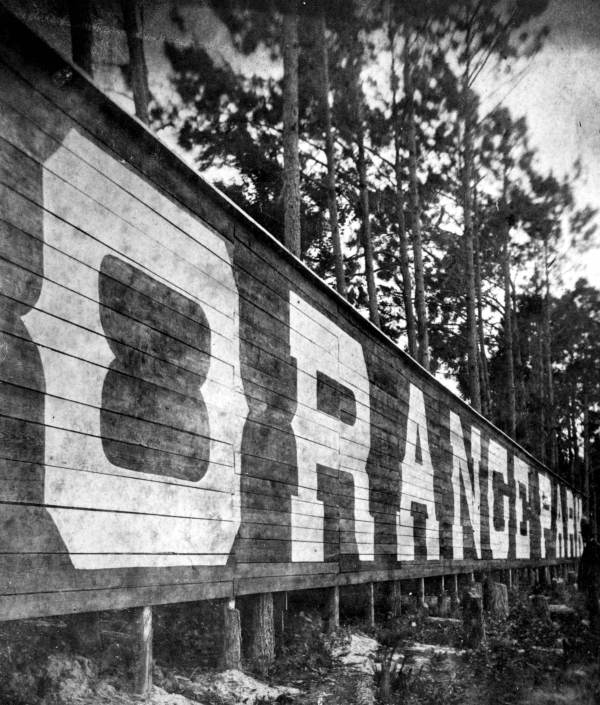
The History of Orange Park, Florida
March 7, 2024The article provides an overview of why Medicare is set at 65, including the historical reasons, eligibility criteria, benefits of enrolling at 65, consequences of delaying enrollment, and the role of employer plans and COBRA. It also highlights the importance of understanding enrollment periods and introduces Green Insurance Agency as a resource for personalized assistance with Medicare enrollment.
Overview of Medicare’s Age Eligibility
The age of 65 was strategically chosen as the Medicare eligibility age due to its alignment with the traditional retirement age in the United States. This alignment was made during the inception of Medicare in 1965, under President Lyndon B. Johnson’s administration, as part of the Social Security Amendments. This decision was based on the context of the time, where 65 was considered a common age for retirement, making it a logical threshold for eligibility for Medicare, a program designed to provide healthcare to the elderly.
Medicare eligibility at 65 allows for a seamless transition from employer-based health insurance to Medicare coverage for many Americans. This transition is crucial as it ensures that individuals who retire at the traditional retirement age continue to have access to healthcare without a coverage gap. The choice of age 65 was also influenced by pre-existing social security benefits which were, and still are, available to individuals starting at age 65, creating a cohesive social support system for older Americans.
The Age of Eligibility
Individuals who have worked and paid Medicare taxes for at least 10 years become automatically eligible for Medicare at age 65, ensuring widespread access to healthcare for seniors. This automatic eligibility is a vital feature of the Medicare system, as it simplifies the enrollment process for millions of Americans each year. For those who have not met the work requirement, options are still available, such as purchasing Medicare coverage, ensuring that all seniors have access to healthcare services.
Medicare eligibility at 65 is also extended to those with certain disabilities who receive Social Security Disability Insurance (SSDI) or Railroad Retirement Board (RRB) benefits. This extension is an important facet of Medicare, as it acknowledges and accommodates individuals who, due to disabilities, may require access to healthcare services before reaching the traditional retirement age.
Benefits of Enrolling at 65
Enrolling in Medicare at 65 provides comprehensive healthcare coverage, including hospital insurance (Part A) and medical insurance (Part B), without the need for additional premiums in most cases. This comprehensive coverage is crucial for seniors, as it covers a wide range of healthcare services, from hospital stays to outpatient services and preventive care. The financial security and peace of mind that come with Medicare coverage cannot be overstated, especially considering the rising cost of healthcare.
Medicare coverage starting at 65 offers peace of mind and financial security, helping individuals manage healthcare costs effectively as they age. The access to a wide range of healthcare services and providers ensures that individuals can maintain their health and well-being throughout their senior years, a significant benefit of enrolling in Medicare at 65.
Consequences of Delaying Enrollment
Delaying Medicare enrollment past age 65 can result in late enrollment penalties, leading to higher premiums for the duration of coverage. These penalties are calculated based on how long an individual delays enrollment, and they can significantly increase the cost of Medicare Part B and Part D premiums. For example, for each 12-month period that enrollment is delayed, the Part B premium may increase by 10%.
Individuals who miss their Initial Enrollment Period may have limited options for enrolling in Medicare and could face gaps in coverage if they delay enrollment. This situation could lead to significant out-of-pocket costs for healthcare services until Medicare coverage begins.
Employer Plans and COBRA
Individuals with employer plans that cover at least 20 employees have the option to delay Medicare Part B enrollment without penalty while still working at 65. This option is a crucial aspect of Medicare’s flexibility, allowing individuals to make choices that best suit their employment and health coverage needs. However, once employment ends, it’s important to enroll in Medicare during the Special Enrollment Period to avoid penalties.
COBRA coverage can impact Medicare enrollment, requiring individuals to sign up for Medicare promptly to avoid coverage gaps and potential penalties. If an individual is covered under COBRA and becomes eligible for Medicare, it’s generally advisable to switch to Medicare to ensure continuous coverage, as COBRA coverage may not be considered creditable coverage for Medicare purposes.
Understanding Enrollment Periods
Special Enrollment Periods provide flexibility for individuals who miss their Initial Enrollment Period due to qualifying events, such as losing employer coverage or relocating. These periods are designed to accommodate life changes and ensure that individuals have access to Medicare coverage when they need it, without facing penalties for late enrollment.
Enrolling in Medicare during the Initial Enrollment Period ensures seamless access to healthcare benefits without incurring late enrollment penalties. This period, which begins three months before the month of an individual’s 65th birthday and ends three months after, is a crucial window for making informed decisions about Medicare coverage.
We’re Here to Help
For personalized assistance with Medicare enrollment, understanding eligibility criteria, and exploring coverage options, contact Green Insurance Agency at (904) 717-1176. Visit Green Insurance Agency to learn more about their services, Medicare offerings, and how they can support you in securing the right healthcare coverage.



